Authors:
Elaine Kong、Kuo-Ting、Huang、Aakash Gautam
Paper:
https://arxiv.org/abs/2408.10108
Introduction
Cancer survivors, particularly those from ethnic and racial minority groups, face significant challenges in their recovery journey. These challenges are often exacerbated by disparities in accessing adequate resources for information and care. Research indicates that as many as half of all cancer survivors suffer from mental health issues such as anxiety, depression, and fear of cancer recurrence. Despite the prevalence of these issues, psychosocial needs are often overlooked within oncological care, signaling a critical area for improvement.
With the advent of Artificial Intelligence (AI), there is growing interest in exploring AI as a solution to bridge these gaps. AI has the potential to provide personalized, culturally aligned, and linguistically appropriate interactions. However, concerns about data privacy, loss of human touch in caregiving, and the risk of echo chambers that limit exposure to diverse information also arise. This study aims to uncover the psychosocial needs specific to cancer survivors and evaluate the potential of AI-based interventions to address these needs.
Related Work
Information-Seeking Behavior During Cancer Journey
Cancer journeys are profoundly individual, and care services need to attend to these personal realities. Research identifies two predominant information-seeking behaviors among cancer patients: active seeking and avoidance. These behaviors shape patient-provider interactions and significantly impact treatment outcomes. Digital platforms are increasingly leveraged by cancer survivors and caregivers to gain health information, with approximately 45% of cancer patients using digital platforms for information.
Personalized Technology Solutions
Scholars have argued for personalized technology solutions that cater to the unique circumstances and needs of cancer survivors and their caregivers. AI-based solutions are positioned as promising tools for improving access to personalized information. However, there are critical gaps in current technologies that need to be addressed to support cancer survivors effectively.
Research Methodology
Data Collection and Analysis
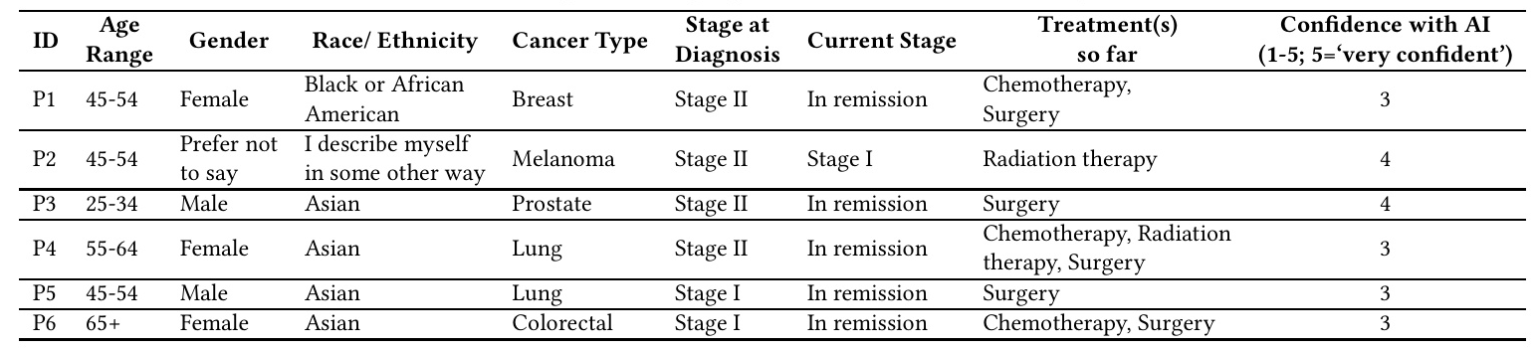
As part of this pilot study, six cancer survivors from diverse backgrounds were interviewed to ensure representation of varied cancer types and stages. The semi-structured interviews, lasting between 45 to 90 minutes, explored participants’ information needs, experiences with healthcare services, sources of community support, and perceptions of using AI in their cancer care journey. Thematic analysis of the transcripts was conducted, starting from open-coding and iteratively working towards higher-level codes. Member checking was conducted to ensure an authentic representation of participants’ ideas.
Experimental Design
Participant Demographics
The study included six participants with diverse backgrounds, cancer types, and stages at diagnosis. The table below provides a summary of the participant demographics:
Interview Structure
The semi-structured interviews focused on exploring participants’ information needs, experiences with healthcare services, sources of community support, and perceptions of using AI in their cancer care journey. The interviews were conducted remotely, considering the participants’ preferences and geographical constraints.
Results and Analysis
Unmet Informational Needs for Their Unique Situation
Participants expressed a wide consensus on the need for transparency about their condition and possible pathways for treatment. Many participants reported increased anxiety about their health and mortality due to a lack of transparency from care providers. In the absence of adequate information from healthcare providers, participants often relied on online resources, which sometimes led to misinformation and increased anxiety.
Need for Personalized Healthcare Services
Participants shared varied experiences with healthcare professionals, noting positive interactions when providers dedicated time to offer personalized care. However, many participants felt neglected or misunderstood by healthcare professionals, highlighting a significant lack of psycho-social support. The burden on healthcare providers and the impersonal nature of technology-mediated interactions were identified as barriers to personalized care.
Seeking Support from Community
Social support from family, friends, and online communities played a pivotal role in providing emotional relief during treatment. Participants emphasized the importance of culturally sensitive interventions that respect and address the distinct needs of various communities. Language barriers were also a significant challenge, with participants seeking support from family members or online groups to navigate these barriers.
Perceived Role of AI in Cancer Support
Participants valued the possibility that AI could provide continuous support, which is hard to get from human services. They envisioned AI helping with personalized health tracking, providing easy-to-understand health resources, and offering immediate support for managing side effects and mental health issues. However, concerns about data privacy, the reliability of AI, and the potential loss of human touch in caregiving were also expressed.
Overall Conclusion
The study highlights the critical gaps in current healthcare systems, particularly in providing personalized, culturally sensitive care for cancer survivors. While AI has the potential to address some of these gaps, significant concerns about data privacy, the reliability of AI, and the potential loss of human touch in caregiving remain. The desire for AI-driven care solutions reflects a deeper issue—the need for control and agency in the face of a malady that erodes both. Addressing these structural problems requires a comprehensive approach that goes beyond technological solutions.
Implications for Future Research
- Personalization and Informed Decision Making: Increasing health literacy and ensuring transparency in AI systems are fundamental in enabling patients to make informed decisions about their treatments.
- Personalization and the Risk of Echo Chambers: AI systems should be designed to introduce patients to a variety of perspectives and options, preventing bias reinforcement and promoting well-rounded, informed decision-making.
- Personalization and Structural Change Trade-off: The primacy of AI solutions risks overlooking the urgent need to address the broader structural issues that impact cancer care and healthcare more generally.
Final Thoughts
Asking “Why personalization?” encourages a participatory approach, bringing cancer care survivors into the design process. Critical health and technology literacy, making available broader sources of information and care, and situating technology in the context of structural issues surrounding healthcare are necessary conditions to support agentic participation in the design process.